Epilepsy
Worrying about your next seizure is no way to live. Our experts can help you find new ways to manage your epilepsy.
Epilepsy
Worrying about your next seizure is no way to live. Our experts can help you find new ways to manage your epilepsy.

Key points about epilepsy
- Refractory epilepsy occurs when your anti-epilepsy medicines are no longer controlling your seizures. Often the cause of refractory epilepsy is not known.
- Your healthcare provider will likely give you other medicines to try to get your seizures under control. If this does not work, other options may be surgery to remove the part of the brain where the seizures start or electrical stimulation of a nerve leading to the brain.
What is epilepsy?
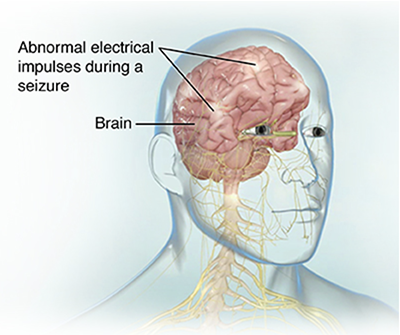
People with epilepsy have seizures. During a seizure, the nerve cells in the brain don't communicate like they should. The usual electrical activity in the brain changes. These seizures may last a few seconds or a few minutes.
Some people with epilepsy will have or will one day develop refractory epilepsy. This means that medicines don't work well, or at all, to control the seizures.
If you have refractory epilepsy, the type of seizures you have may affect your treatment. Seizures may be:
- Primary (generalized) seizures. This means they involve both sides of your brain.
- Partial (focal) seizures. This means seizure activity starts in a smaller part of your brain. It may later spread out to a wider area.
Refractory epilepsy can have a big effect on your life. People with this type of epilepsy may have trouble at work or school. They may worry a lot about when their next seizure will come. They may also have injuries that result from their seizures. If your healthcare provider thinks you have refractory epilepsy, he or she may suggest that you visit a medical center that specializes in epilepsy.
What are the symptoms of epilepsy?
The symptoms of a seizure can include:
- Convulsions, or shaking movements
- Loss of consciousness
- Confusion
- Tongue biting
- Lip smacking
- Loss of bowel or bladder control
- Uncontrolled eye movements
- Staring into space
- Falling
- Muscle rigidness, tremors, or twitching
- Odd behavior (such as screaming or yelling)
If you still have seizures while you're taking medicine for them, you may have refractory epilepsy.
When should I contact my doctor?
Seek care immediately if:
- You have a seizure that lasts for more than five minutes.
- This is the first time you've experienced a seizure.
- You remain unconscious after having a seizure.
- You sustain a serious injury during a seizure or if you have trouble breathing.
Call your doctor and request an appointment within the next 24 hours if:
- You continue to have seizures despite taking your medication.
- Your seizures become worse in intensity or frequency.
- You have new symptoms during or after your seizures.
Epilepsy care at UW Medicine
At UW Medicine, you have access to teams of diverse specialists who are passionate about caring for their patients and are also involved in research. We have specialists in adult and pediatric neurology, neurosurgery, neuroradiology, neuropathology and neuropsychology, as well as nurses, social workers, vocational rehabilitation specialists and electrodiagnostic technicians. Our clinicians take the time to understand your needs and walk you through the risks and benefits of any treatment path.
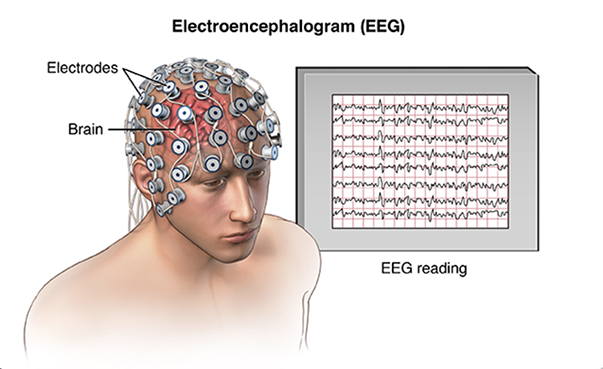
You'll see a neurologist who specializes in epilepsy during your first visit. You may undergo monitoring using video electroencephalogram (EEG) and brain-imaging techniques to determine the underlying causes of your ongoing seizures. Then, an entire team of clinicians reviews your data to recommend the best treatments to allow you to return to your normal life.
Your treatment may involve medication or minimally invasive neurosurgical procedures. Your UW Medicine care team will work with you every step of the way, no matter which treatment you choose. At the Regional Epilepsy Center at Harborview, focused research also means you have access to innovative therapies and treatments.
Nationally recognized for epilepsy treatment
UW Medicine doctors specializing in epilepsy
Andrea L. Cheng-Hakimian M.D.
Medical Specialties
John Christopher Oakley M.D., Ph.D.
Medical Specialties
Appointments
206.598.7688Nicholas Pete Poolos, MD, PhD
Medical Specialties
UW Medicine locations specializing in epilepsy
Neurology Clinic at UW Medical Center - Montlake
Medical Specialties
Hours Today
Regional Epilepsy Center at Harborview
Medical Specialty
Hours Today
What causes epilepsy?
Some seizures have known causes, such as head injuries, infections, fevers, or brain tumors. But often the cause of seizures in epilepsy is not known.
In the same way, it is not clear why some people with epilepsy are not helped by anti-epilepsy medicines. Or why these medicines sometimes stop working. The electrical activity in the brain during a seizure might get so high that medicines are no longer able to control it. But why this happens is not known.
How is epilepsy diagnosed?
Your healthcare provider will likely ask you many questions about your seizures. You will likely also have a test called an electroencephalogram (EEG). This involves placing electrodes on your scalp to measure your brain's activity. Sometimes, the EEG can be watched for long spans of time at home or in the hospital.
Your healthcare provider may also want you to have a CT or MRI scan of your brain. If you eventually need surgery to treat the problem, your healthcare provider may do more tests like these to find out where your seizures are starting.
You will need to work closely with your healthcare provider to find out whether your epilepsy is refractory. Your provider may need to watch you closely during more seizures to try several medicines before he or she feels your condition is refractory. Your healthcare provider may want you to check in often to report your symptoms as you try different medicine doses.
How is epilepsy treated?
Your healthcare provider may suggest that you take other anti-epilepsy medicine. You may take it alone or with others you are already taking. There are many different medicines in this class. Some that may be tried are:
- Carbamazepine
- Phenytoin
- Neurontin
- Lamotrigine
- Levetiracetam
- Oxcarbazepine
- Tiagabine
- Topiramate
- Zonisamide
If medicines aren't helping with your seizures, you may need:
- Surgery. Surgery may be very helpful if you have refractory partial epilepsy and the part of the brain where the seizures start can be found and safely removed. Your healthcare provider may advise surgery if you still have seizures after trying several anti-epilepsy medicines. During the procedure, the healthcare provider will take out the part of your brain that's starting the seizures.
- Electrical stimulation. If you can't have or don't want brain surgery, your healthcare provider may suggest vagus nerve stimulation (VNS) with an implantable device. The device is placed under your skin in your chest. Wires connect it to the vagus nerve in your neck. It sends a current to the nerve. With this device, you may have fewer seizures. It may also help lessen the severity of a seizure that has already started.
Living with epilepsy
Living with refractory epilepsy can be hard. People with this health problem may worry a lot about when their next seizure will come. They may have trouble at work or school. They may no longer be allowed to drive. They may also have injuries that result from their seizures. It is important to do what you can to limit your chances of injury.
A special diet called a ketogenic diet may help control your seizures. This type of diet is high in fats and low in carbohydrates. If you follow this diet, you will need to work closely with your healthcare provider and take supplements of certain nutrients as needed.